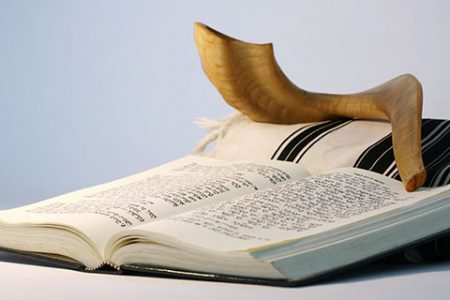
On Yom Kippur, the Day of Atonement, as Jews the world over confront the uncertainty of their personal futures and chant the somber holiday prayer Unetaneh Tokef affirming a higher power’s mandate to decide who shall die and how, new research, led by the Hadassah Medical Center’s Intensive Care Unit Director Emeritus Prof. Charles Sprung reveals a significant change in physicians’ attitudes toward end-of-life interventions in the intensive care units (ICUs) of Europe and Israel.
The study, appearing in the October 2 online Journal of the American Medical Association (JAMA), compares data from 1999-2000 with that from 2015-2016 regarding end-of-life intervention in 22 intensive care units. The international research team found that even in more conservative countries in Southern Europe and in Israel, doctors are less likely to use radical interventions to extend life. Physicians are no longer viewing death as their failure and are changing their approach to keeping patients alive.
“Whereas before they tended to use methods with limited success rates to try and prolong life,” Prof. Sprung says, in more recent years, “there has been more openness in discussing end-of-life issues and a change in consensus.” He explains, “As time has progressed, certainly in intensive care, we realize that having a patient die isn’t a failure. You do whatever you can to save patients but when a time comes where you cannot save them, giving them palliative care so they don’t suffer is extremely important not only for the patients but also for the families.”
The JAMA article highlights the statistical changes that have occurred. At the 22 centers participating in this study, 1,785 patients comprised the study population for 2015-2016. In 1999-2000, 2,807 patients made up the study sample. Patients were followed until discharge from the ICU, death, or two months from the first decision to limit life-prolonging therapies. In 2015-2016, the researchers determined, 89.7 percent of the physicians did not insist on life-prolonging interventions versus 68.3 percent 16 years ago.
In arriving at their conclusions, the researchers looked at limitations in life-prolonging therapy, including withholding or withdrawing of life-prolonging treatment, as well as shortening the dying process. Withholding treatment included such decisions as not to perform cardiopulmonary resuscitation if a patient went into cardiac arrest. Withdrawing treatment included such decisions as actively stopping a norepinephrine infusion, aimed at preventing shock. Active shortening of the dying process involved someone performing an act with the specific intent to shorten the dying process.
To the researchers’ surprise, an outcome of this shift in approach was that the decision not to place a patient on a ventilator or intervene in other ways proved fatal less often than they would have thought, providing a certain relief to the physicians who struggle with these decisions. Specifically, survival after any therapy limitation was significantly higher in 2015-2016 (20.4 percent) than in 1999-2000 (5.5 percent). The improved 2015-2016 survival rate was present in all three regions. The authors hypothesize that this reflects improved ICU practices, with more patients surviving acute illnesses.
As Prof. Sprung says, “The interesting discovery that withholding intervention doesn’t mean that a patient will die relieves some of the weight of the decision for families as well as for hospital staff.”
The research team divided Europe into three regions—northern (Denmark, Ireland, the Netherlands, and the United Kingdom), central (Belgium, Czech Republic, Germany, and Switzerland), and southern (Greece, Israel, Italy, Portugal, Spain, and Turkey). Some differences were found among the three regions. In Southern European countries and Israel, ICU staff and families were more likely to opt for cardiopulmonary resuscitation, ventilation, and other life-prolonging strategies. Doctors in Northern Europe decided more rapidly whether or not to use therapies to extend the life and were less inclined to demand the full range of life-extending interventions. Nevertheless, although those nuances persisted, all three regions followed the trend to limit life-extending interventions.
Prof. Sprung presented these study findings at the European Society for Intensive Care Medicine’s annual congress in Berlin, Germany, on October 2.
Link to JAMA article https://jamanetwork.com/journals/jama/fullarticle/2752581
